 Research at the UKE?
Research at the UKE?
Friese Lab – Neuroimmunology and Multiple Sclerosis
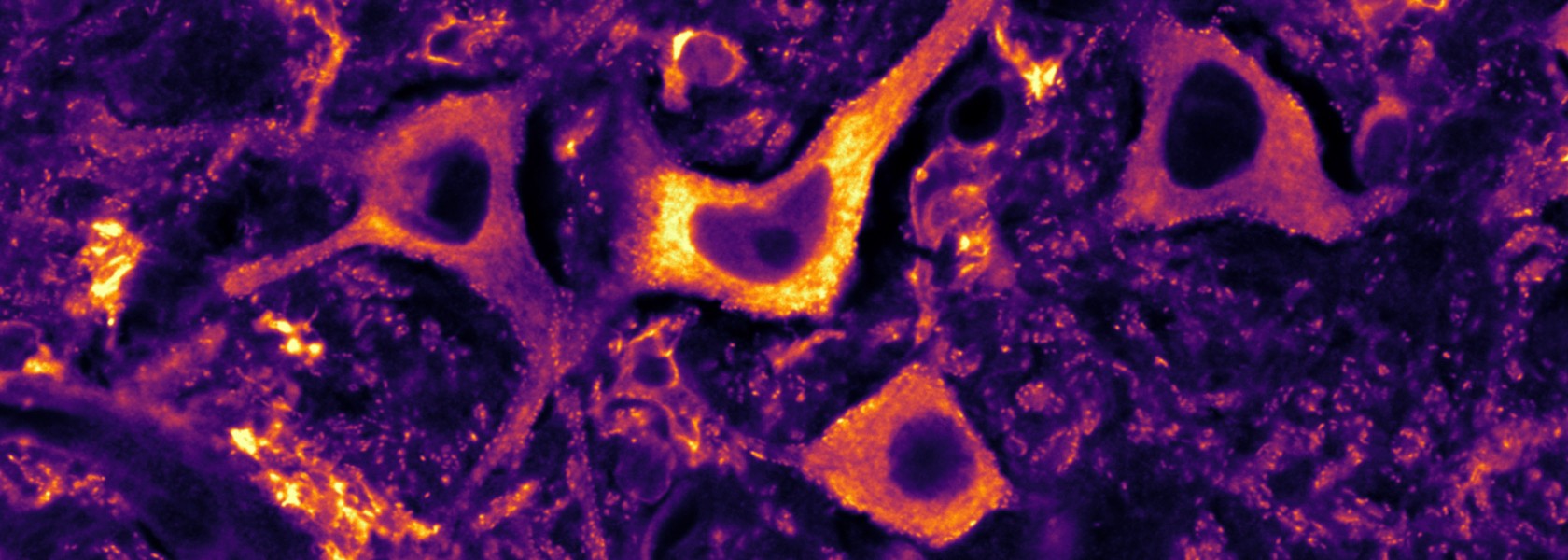
The aetiology and pathogenesis of multiple sclerosis and other neuroimmunological or neuroinfectious diseases remains largely unknown. In order to design more efficacious treatments, we investigate the immune and the nervous system and their interactions to understand mechanisms of immune cell dysregulation and neurodegeneration.
“Understating neuro-immune interactions to halt inflammation-induced neurodegeneration.”
Prof. Dr. Manuel Friese
Project details and goals
We seek to better understand the development and progression of neuroimmunological and neuroinfectious diseases with particular emphasis on multiple sclerosis to translate molecular findings into drug treatment and improve clinical care. In order to achieve this goal, we systematically study immunology, neurobiology and patient care using a wide methodological spectrum.
- How is an autoimmune response generated?
- How does sex difference and pregnancy modulate multiple sclerosis disease activity?
- How do neurons react to inflammatory stressors and degenerate?
- How do infections of the central nervous system result in immunopathology?
- Which proteins are suitable drug targets to halt inflammation-induced neurodegeneration?
Key Publications – Friese Lab
Woo MS*, Mayer C*, Binkle-Ladisch L, Sonner JK, Rosenkranz SC, Shaposhnykov A, Rothammer N, Tsvilovskyy V, Lorenz SM, Raich L, Bal LC, Vieira V, Wagner I, Bauer S, Glatzel M, Conrad M, Merkler D, Freichel M, Friese MA. STING orchestrates the neuronal inflammatory stress response in multiple sclerosis. Cell. 2024; 187:1-18. *both authors con-tributed equally.
Abstract:
Inflammation-induced neurodegeneration is a defining feature of multiple sclerosis (MS), yet the underlying mechanisms remain unclear. By dissecting the neuronal inflammatory stress response, we discovered that neurons in MS and its mouse model induce the stimulator of interferon genes (STING). However, activation of neuronal STING requires its detachment from the stromal interaction molecule 1 (STIM1), a process triggered by glutamate excitotoxicity. This detachment initiates non-canonical STING signaling, which leads to autophagic degradation of glutathione peroxidase 4 (GPX4), essential for neuronal redox homeostasis and thereby inducing ferroptosis. Both genetic and pharmacological interventions that target STING in neurons protect against inflammation-induced neurodegeneration. Our findings position STING as a central regulator of the detrimental neuronal inflammatory stress response, integrating inflammation with glutamate signaling to cause neuronal cell death, and present it as a tractable target for treating neurodegeneration in MS.
Rothammer N, Woo MS, Bauer S, Binkle-Ladisch L, Di Liberto G, Egervari K, Wagner I, Haferkamp U, Pless O, Merkler D, Engler JB, Friese MA. G9a dictates neuronal vulnerability to inflammatory stress via transcriptional control of ferroptosis. Sci Adv. 2022 Aug 5;8(31):eabm5500.
Abstract:
Neuroinflammation leads to neuronal stress responses that contribute to neuronal dysfunction and loss. However, treatments that stabilize neurons and prevent their destruction are still lacking. Here, we identify the histone methyltransferase G9a as a druggable epigenetic regulator of neuronal vulnerability to inflammation. In murine experimental autoimmune encephalomyelitis (EAE) and human multiple sclerosis (MS), we found that the G9a-catalyzed repressive epigenetic mark H3K9me2 was robustly induced by neuroinflammation. G9a activity repressed anti-ferroptotic genes, diminished intracellular glutathione levels, and triggered the iron-dependent programmed cell death pathway ferroptosis. Conversely, pharmacological treatment of EAE mice with a G9a inhibitor restored anti-ferroptotic gene expression, reduced inflammation-induced neuronal loss, and improved clinical outcome. Similarly, neuronal anti-ferroptotic gene expression was reduced in MS brain tissue and was boosted by G9a inhibition in human neuronal cultures. This study identifies G9a as a critical transcriptional enhancer of neuronal ferroptosis and potential therapeutic target to counteract inflammation-induced neurodegeneration.
Kaufmann M, Evans H, Schaupp AL, Engler JB, Kaur G, Willing A, Kursawe N, Schubert C, Attfield KE, Fugger L, Friese MA. Identifying CNS-colonizing T cells as potential therapeutic targets to prevent progression of multiple sclerosis. Med. 2021 Mar 12;2(3):296-312.e8.
Abstract:
Background: Multiple sclerosis (MS), an autoimmune disease of the central nervous system (CNS), can be suppressed in its early stages but eventually becomes clinically progressive and unresponsive to therapy. Here, we investigate whether the therapeutic resistance of progressive MS can be attributed to chronic immune cell accumulation behind the blood-brain barrier (BBB).
Methods: We systematically track CNS-homing immune cells in the peripheral blood of 31 MS patients and 31 matched healthy individuals in an integrated analysis of 497,705 single-cell transcriptomes and 355,433 surface protein profiles from 71 samples. Through spatial RNA sequencing, we localize these cells in post mortem brain tissue of 6 progressive MS patients contrasted against 4 control brains (20 samples, 85,000 spot transcriptomes).
Findings: We identify a specific pathogenic CD161+/lymphotoxin beta (LTB)+ T cell population that resides in brains of progressive MS patients. Intriguingly, our data suggest that the colonization of the CNS by these T cells may begin earlier in the disease course, as they can be mobilized to the blood by usage of the integrin-blocking antibody natalizumab in relapsing-remitting MS patients.
Conclusions: As a consequence, we lay the groundwork for a therapeutic strategy to deplete CNS-homing T cells before they can fuel treatment-resistant progression.
Funding: This study was supported by funding from the University Medical Center Hamburg-Eppendorf, the Stifterverband für die Deutsche Wissenschaft, the OAK Foundation, Medical Research Council UK, and Wellcome.
Woo MS, Ufer F, Rothammer N, Di Liberto G, Binkle L, Haferkamp U, Sonner JK, Engler JB, Hornig S, Bauer S, Wagner I, Egervari K, Raber J, Duvoisin RM, Pless O, Merkler D, Friese MA. Neuronal metabotropic glutamate receptor 8 protects against neurodegeneration in CNS inflammation. J Exp Med. 2021 May 3;218(5):e20201290.
Abstract:
Multiple sclerosis (MS) is a chronic inflammatory disease of the central nervous system with continuous neuronal loss. Treatment of clinical progression remains challenging due to lack of insights into inflammation-induced neurodegenerative pathways. Here, we show that an imbalance in the neuronal receptor interactome is driving glutamate excitotoxicity in neurons of MS patients and identify the MS risk–associated metabotropic glutamate receptor 8 (GRM8) as a decisive modulator. Mechanistically, GRM8 activation counteracted neuronal cAMP accumulation, thereby directly desensitizing the inositol 1,4,5-trisphosphate receptor (IP3R). This profoundly limited glutamate-induced calcium release from the endoplasmic reticulum and subsequent cell death. Notably, we found Grm8-deficient neurons to be more prone to glutamate excitotoxicity, whereas pharmacological activation of GRM8 augmented neuroprotection in mouse and human neurons as well as in a preclinical mouse model of MS. Thus, we demonstrate that GRM8 conveys neuronal resilience to CNS inflammation and is a promising neuroprotective target with broad therapeutic implications.
Schattling B, Engler JB, Volkmann C, Rothammer N, Woo MS, Petersen M, Winkler I, Kaufmann M, Rosenkranz SC, Fejtova A, Thomas U, Bose A, Bauer S, Träger S, Miller KK, Brück W, Duncan KE, Salinas G, Soba P, Gundelfinger ED, Merkler D, Friese MA. Bassoon proteinopathy drives neurodegeneration in multiple sclerosis. Nat Neurosci. 2019 Jun;22(6):887-896.
Abstract:
Multiple sclerosis (MS) is characterized by inflammatory insults that drive neuroaxonal injury. However, knowledge about neuron-intrinsic responses to inflammation is limited. By leveraging neuron-specific messenger RNA profiling, we found that neuroinflammation leads to induction and toxic accumulation of the synaptic protein bassoon (Bsn) in the neuronal somata of mice and patients with MS. Neuronal overexpression of Bsn in flies resulted in reduction of lifespan, while genetic disruption of Bsn protected mice from inflammation-induced neuroaxonal injury. Notably, pharmacological proteasome activation boosted the clearance of accumulated Bsn and enhanced neuronal survival. Our study demonstrates that neuroinflammation initiates toxic protein accumulation in neuronal somata and advocates proteasome activation as a potential remedy.
Further information about Friese Lab
Further information about the Friese laboratory can be found on the website of the Institute of Neuroimmunology and Multiple Sclerosis (INIMS).